The Menopause Issue!
Hello!
Dear Patient,
Happy summer to all! I am so glad to see the return of longer days and (finally!) warmer weather. I hope you’re making plans to enjoy some quality time outdoors.
I would like to focus this newsletter on perimenopause and menopause, as I feel that more and more patients are coming in with questions regarding this “Change of Life.”
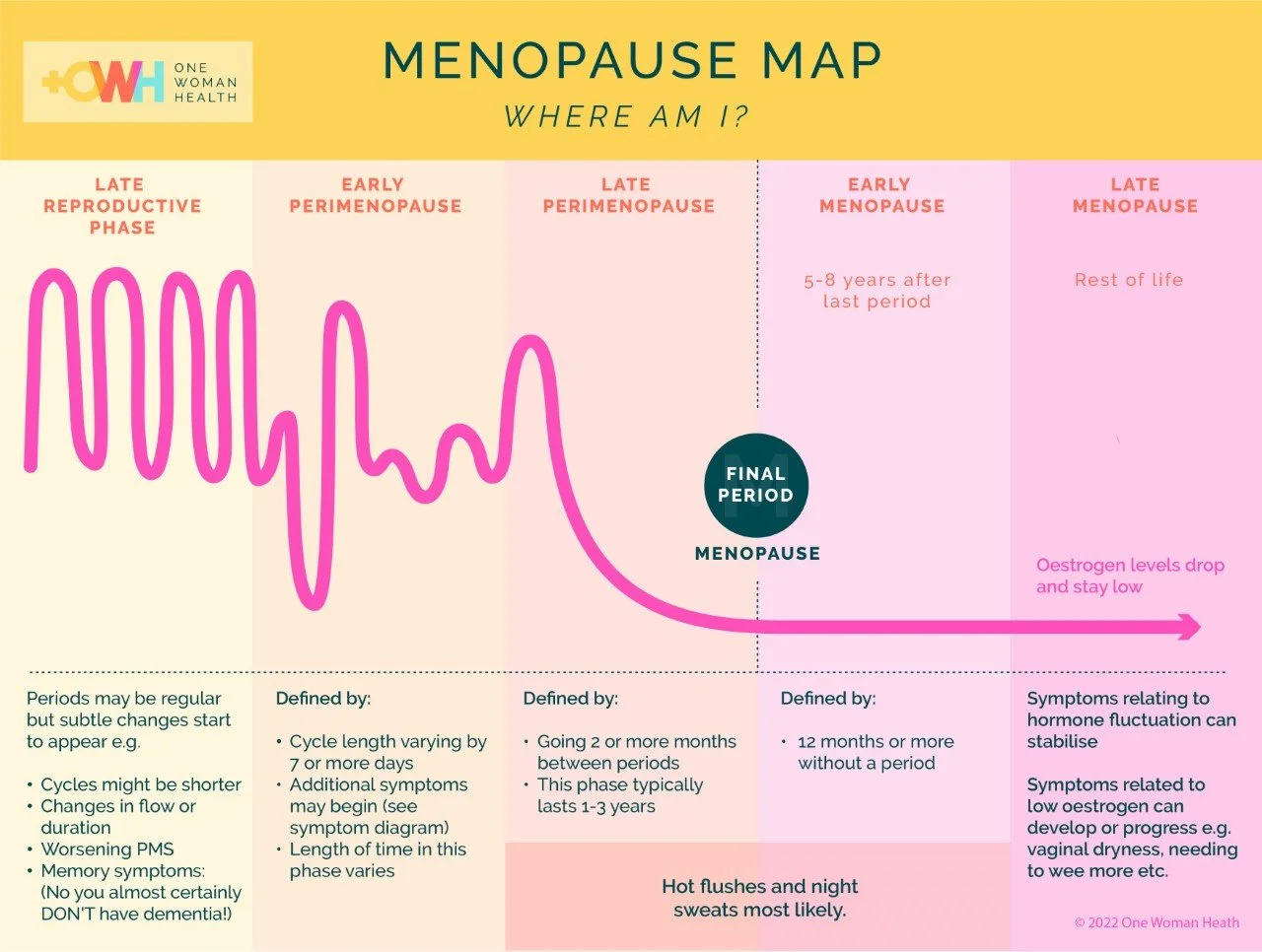
What exactly does it entail? Menopause, by definition, marks 12 calendar months without a period. In the US, the average age for this is 51 years old. The 5 to 10 years surrounding menopause is called perimenopause. It’s when estrogen production by the ovaries gradually declines, leading to a range of symptoms.
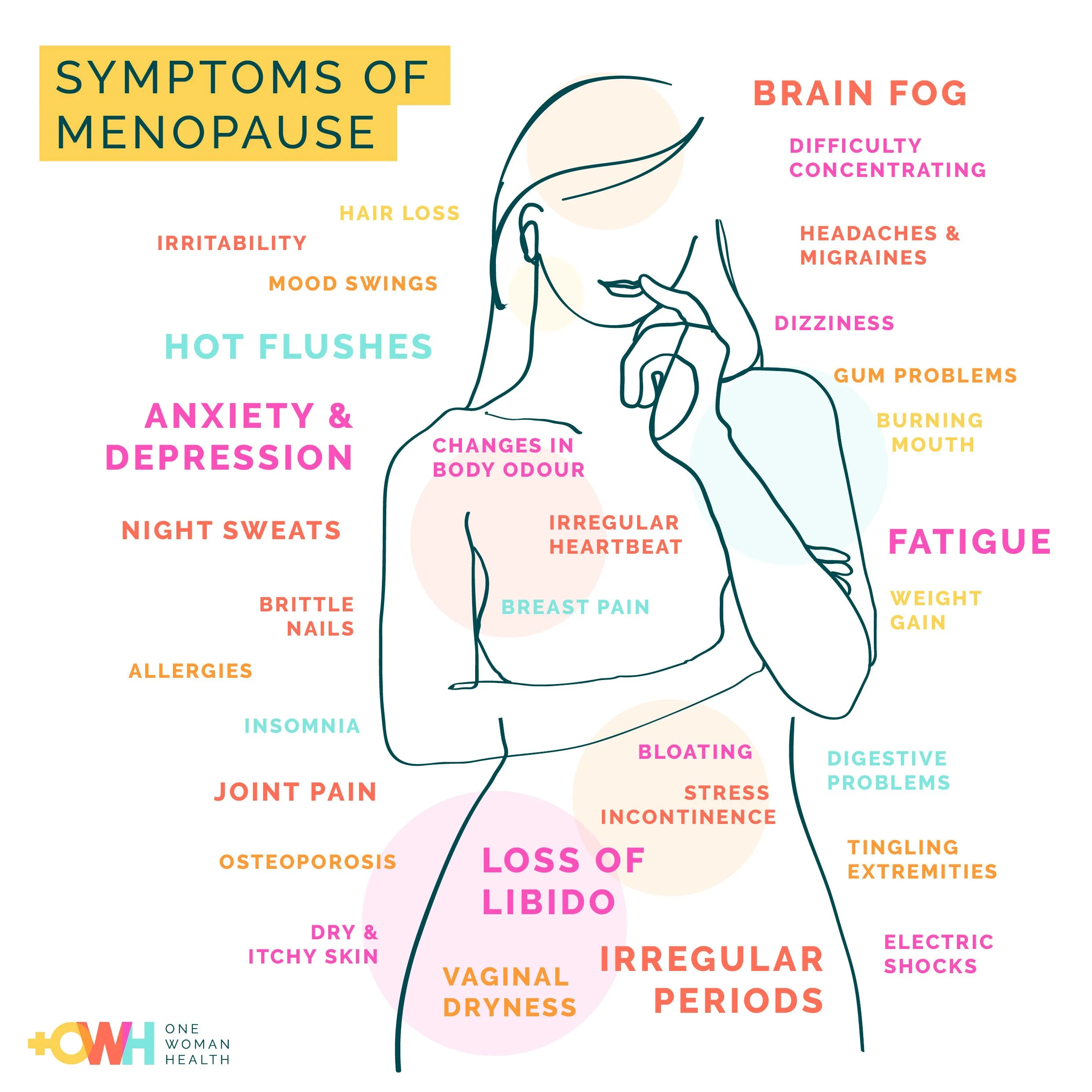
Chances are, most women in their early 40s onward will deal with some perimenopausal symptoms. To describe the breadth of symptoms, let’s go back to the basics. Which parts of our bodies contain estrogen receptors? As it turns out, almost all!
—Dr. Sogol Jahedi
The Ups and Downs Are Real.
In the perimenopausal transition, estrogen declines in an erratic manner. Some months the ovaries produce the usual amounts and everything feels fine. During others, there is less produced and symptoms become bothersome. For some women, bothersome is an understatement. Symptoms can be fully disruptive to quality of life! I tell my patients that the menopausal transition is like pregnancy: Every woman experiences it differently. Some lucky women glide through with no issues. Others are just miserable. Most are somewhere in between. There is no justice in the timeline of this process—these changes take place over years, waxing and waning until periods finally stop. Hot flashes can continue for up to a decade after your last menstrual period.
Patients come to me with a host of concerns:
Weight gain. The #1 complaint! This weight seems to come on no matter how carefully you’re monitoring diet and increasing exercise. And it settles right around the middle.
Hot flashes and night sweats. Daytime hot flashes make it hard to give a presentation to a roomful of colleagues, causing women to become self-conscious in the workplace. The night sweats cause nighttime awakening, which then leads to the next symptom…
Insomnia and fatigue. Women don’t have trouble falling asleep—the trouble is staying asleep. After a nighttime awakening at 2–3 a.m., most women are up for an hour or two, falling back asleep just as the morning alarm goes off. Which then leads to…
Irritability. You’re exhausted! Is it any wonder you’re on a shorter fuse? I commonly hear apologies for how short someone is with their partner and kids, but they can’t help it. Women know that they are not feeling their usual selves.
Increased anxiety. Women without previous anxiety now report feeling anxious. Women with a history of anxiety feel it has increased a lot.
And more! Brain fog, heart palpitations, joint pain, decreased libido, vaginal dryness, painful intercourse, heavy periods, etc.
I have a friend and colleague (thanks, Dr. Flowers!) who jokes that there is a reason it is called the Change of Life. Not a change of mood or a change in health. This is a life-altering passage. You’re not quite the same person afterward! Hormones are powerful.
Lots of Problems. Any Answers?
For all these symptoms, what is there to do? The short answer is, it depends on the individual woman and her situation. First up, lifestyle modifications:
Weight gain. Studies show that estrogen stimulates muscle cells, and decreasing estrogen leads to decreasing muscle mass. Since muscles are calorie-burning tissue, weight gain inevitably follows. But more resistance training can help regain muscle mass.
More exercise. A good weekly goal is at least 150 minutes of moderate exercise and two sessions of strength training.
Intentional eating patterns. Aging leaves less wiggle room for poor food choices. Put bluntly, you cannot get away with having french fries all of the time the way you did in your 20s or 30s! Focus on healthy food choices, especially plant-based, beneficial fats and fiber.
I often advise medical therapies at the very same visit. It’s not an either/or choice:
Menopausal hormone therapy with transdermal estrogen has proved safe and effective for most women. Menopause medicine has progressed a lot since results of the long-term Women’s Health Initiative study were released in 2000. Much of what we first believed about hormonal treatment has been modified.
Numerous non-hormonal options including SSRIs (Paxil), SNRIs (Effexor), gabapentin (Neurontin) and Fezolinetant (Veozah) can be effective in treating hot flashes.
Mind-body approaches like acupuncture, cognitive behavioral therapy and mindfulness-based stress reduction can reduce the severity of hot flashes.
The options are far more than one newsletter can cover. The Menopause Society has great patient information, including a wealth of special-topic videos. Or come on in to discuss!
Menopause: the Novel?
I usually prescribe medicines, not books, but Miranda July’s All Fours made so many “best of” lists that I’ll make an exception. Critics are hailing it as the first novel about perimenopause. It was fantastic! Surely it’s no mistake that the cover’s cliff resembles a graph of falling estrogen levels. To quote one review, “July’s candor, her fearlessness, in describing the unwieldy emotional and biological nuances of this time of life is refreshing.…As a so-called woman of a certain age, I felt seen in a way that is rare.”
From Greta, our Office Manager
Please bear with us while we undergo a change in billing software this month. We are working hard to make this a seamless process for you. As always, if there is any confusion or questions about your statements or billing, feel free to call us to clarify.
Membership Fee Increase
We are grateful to you for choosing Advanced Gynecology for your care. We want to maintain a safe space in this broken healthcare system where all patients feel heard and respected. Unfortunately, costs like medical supplies, billing, electronic medical records and credit-card processing keep rising, while insurance reimbursements are nearly flat. That’s why we find it necessary to increase the membership fee to $500/year (or $45/month) as of July 15, 2025. This is the first increase since late 2021, when our membership program began.
Better Pain Control
In May, the American College of Obstetrics and Gynecology issued much-anticipated pain-management recommendations for office procedures like colposcopy, endometrial biopsy, hysteroscopy and IUD insertions.
In fact, Advanced Gynecology has been using many of these new recommendations for the past 10 years! We reduce the pain of IUD insertions, for example, with cervical-softening agents and both topical and injectable lidocaine.
Still, some patients need more to reduce pain and anxiety. In keeping with our focus on patient comfort, we are considering offering in-office nitrous oxide (“laughing gas”) in addition. Though nitrous sedation is common at dental offices, medical insurance doesn’t cover it for gynecologic procedures. The out-of-pocket costs for this patient-controlled analgesia would be approximately $150–200. Interested in this option if you need a procedure? We are trying to gauge demand, so let us know using the survey below!
A Member Writes
“Doctors like Dr. Jahedi don’t really seem to exist anymore. She sees you as a whole person who deserves her time and expertise rather than a 15-minute block on an overfilled schedule. You get concierge-level care without paying tens of thousands of dollars for a visit.”
—Kelly H., patient