The Breast Cancer Issue
Happy fall, y’all!
I hope everyone had a lovely summer! Summer is my favorite season, so it’s hard for me to see it wind down. September has arrived, however, with the return to school (for some) and, for most, an uptick in the pace of life. I wish you well as the season starts, but hope you can eke out some last summer living during this Labor Day weekend!
I want to dedicate this issue to breast cancer awareness. October is breast cancer awareness month, which has been recognized in the United States now for four decades.
—Dr. Sogol Jahedi
Breast 101
Breast cancer screening is a big part of what we do at Advanced Gynecology, and there is a lot to know. Let’s start with the anatomic basics.
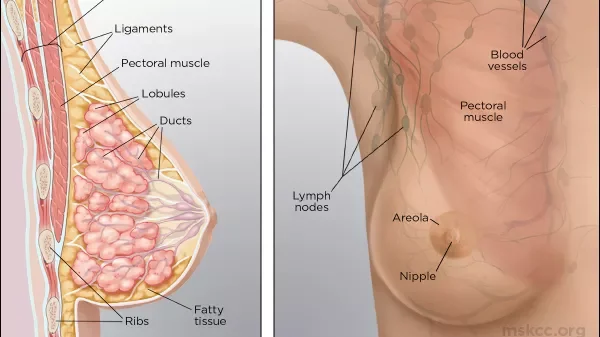
Breast tissue is composed of lobules (small round sacs that produce milk) and milk ducts (canals that carry milk from the lobules to the nipple openings during breastfeeding).
• Lobules are small, round sacs that make milk. We call breast cancer that starts in this tissue lobular cancer.
• Ducts are thin tubes that carry milk to the nipple openings during breastfeeding. Cancers that start here we call ductal cancer. This is the most common type of breast cancer.
• Fibrous tissue is also called connective tissue. Fatty tissue fills the space between your lobules and ducts. Some rare forms of breast cancer start in fibrous and fatty tissue.
• Lymph nodes are small organs in your armpit, collarbone, neck, and chest. Sometimes, breast cancer can spread to lymph nodes.
All about Mammograms
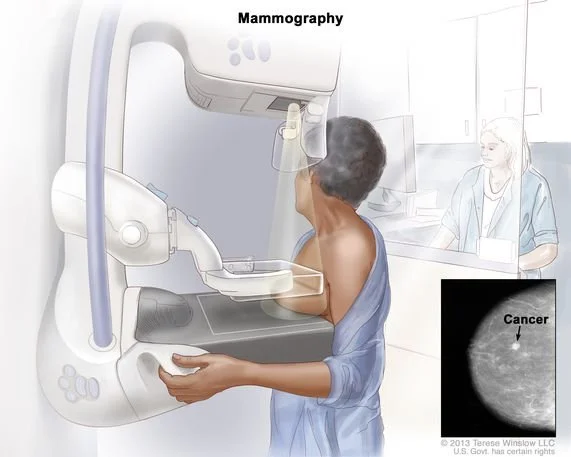
As you probably know, we use screening mammograms to check for breast cancer. A mammogram is just an x-ray of the breast. Most mammography is done with digital breast tomosynthesis (DBT)—also called 3D mammography. Here, computer software combines multiple 2-dimensional, digital breast x-rays to create a 3D image.
Age 40 is the usual time to begin screening. The American Cancer Society (ACS) states that women ages 40–44 should have the option of an annual mammogram—so most insurance must cover it with no cost to you. The ACS recommends screening mammography every year starting at age 45, and every 1–2 years for women ages 55 and up.
Some women may need earlier screening—or more extensive screening with MRI—based on their personal risk factors or family histories. We will discuss this together at your annual exam.
I always tell my patients that a first mammogram, especially, may generate a callback for more images. Please don’t assume the worst! This first mammogram establishes a baseline for you; future testing will compare new images to this baseline to identify changes.
When Mammograms Aren’t Enough
For many women, the screening mammograms note “dense breast tissue.” For them, the recommendation is a screening breast ultrasound. Dense breast tissue increases your risk of a breast cancer —and makes it hard for a radiologist to spot one by mammogram alone. Ultrasound can often find such abnormalities. Financial note: Frustratingly, insurance coverage of screening ultrasounds hasn’t been uniform by state or by insurer. I’m glad to share that an 2026 update to the Affordable Care Act requires that this imaging be at no patient cost, just like mammograms.
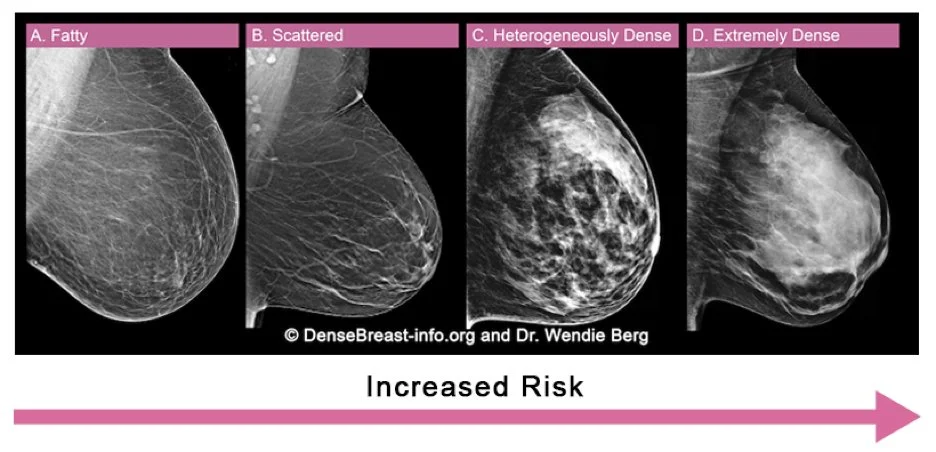
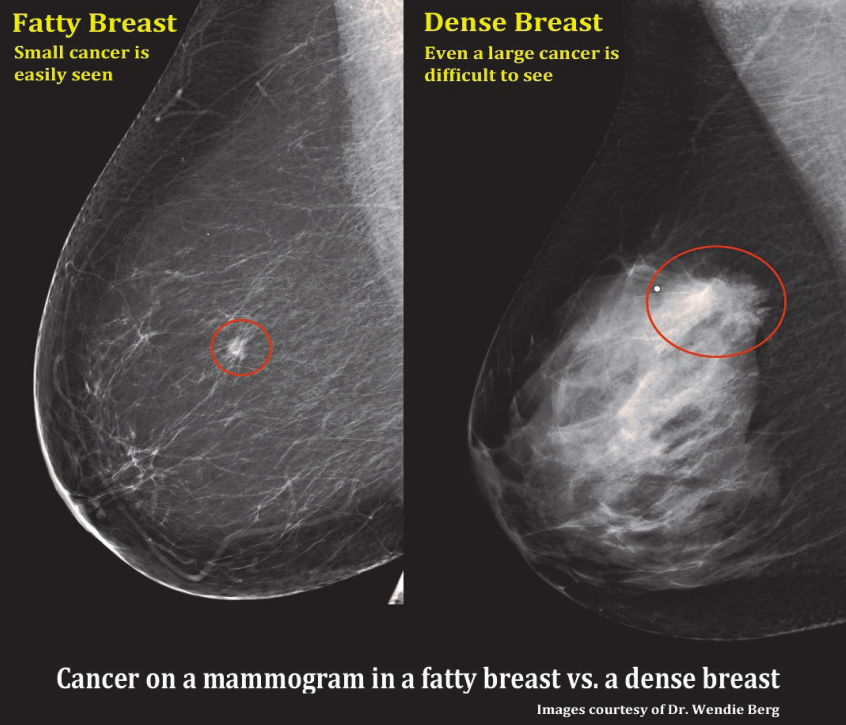
In every mammogram report, breast tissue is categorized from A to D:
A cancer shows up as white on mammogram, as does dense breast tissue. A picture is worth a thousand words—in this case, demonstrating how much harder it is to see a breast cancer in dense breast tissue!
Risks We Face,
Actions to Take
It seems like everyone knows someone who is in treatment for breast cancer. It can be scary to watch a loved one go through this diagnosis and the associated treatments. The experience often leads to (very understandable!) worry about whether we are doing everything we can to avoid the same fate.
So what determines your risk? You have several components:
Genetics. Your family history plays a role. A dozen or so genes predispose us to breast cancer, with the most well known being BRCA1 and BRCA2. A genetic testing panel offered in our office through Invitae Laboratories can test for these and other high-risk genes. Ask us for more information if you are interested.
Age. In addition to being born female, age is the biggest risk factor for breast cancer. We can’t do anything about getting older, other than remember that aging is a privilege we all want to have!
Lifestyle. This one is a modifiable! Being overweight or obese after menopause; drinking alcohol; or taking certain (but not all!) menopausal hormone therapy can increase your risk of breast cancer. Smoking, too, may increase risk. Researchers have identified an impressive list of factors, with many more being studied.
Fortunately, some factors can decrease your breast cancer risk:
Exercise/physical activity
Fruits and vegetables, specifically carotenoids. These are natural, orange-red pigments found in fruits and vegetables such as melons, carrots and sweet potatoes. Dark, leafy green vegetables such as broccoli, spinach and kale also contain carotenoids.
Breastfeeding
Heavier body weight before before menopause. (Excess weight after menopause, however, increases breast cancer risk.)
Despite it all, cancer frequently happens for reasons that we don’t understand and cannot explain. The best path forward is educating yourself and partaking in breast cancer screening. Come in for a clinical breast exam once a year. Make sure that you get your annual mammogram. Do your best to lead a healthy and active lifestyle. You can only do what you can…but you can do a lot!
Fall Immunizations
An update for those lucky enough to have avoided all the clamor: The world of immunizations has seen big changes this year. How will they affect you?
In the fall, we always offer and recommend a flu shot for everyone. This year, like always, we’ll stock these vaccines. And, like always, the versions we stock are thimerisol-free.
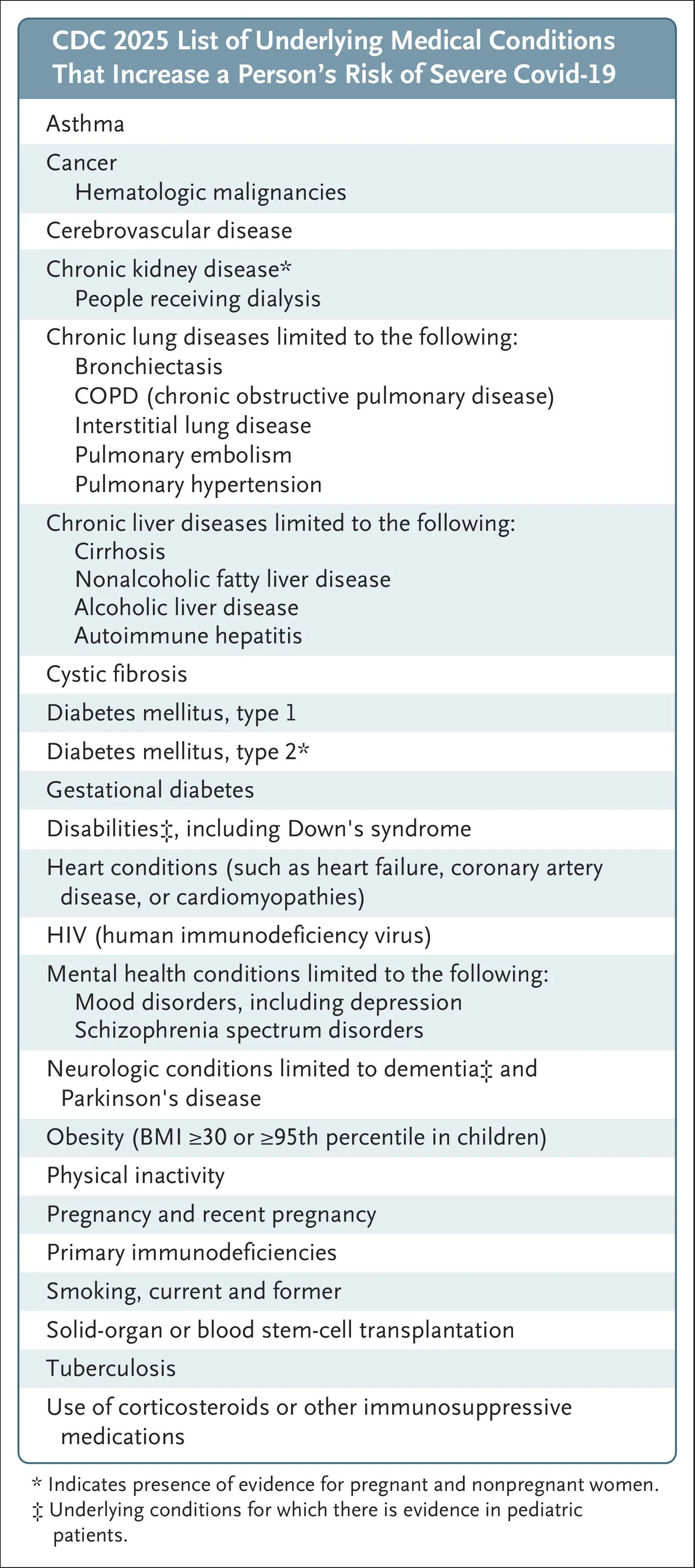
For the Covid-19 vaccine, some things changed and others did not. Manufacturers will still create a fall booster to match the virus’s latest, most common strains. And people at high risk for severe Covid-19 — like those over 65, immunocompromised individuals, and healthcare workers — are still recommended to get this updated booster if it’s been over 12 months since their last vaccination.
As of July, however, the CDC no longer recommends routine Covid-19 vaccination for healthy adults under 65 years of age.
The catch here is knowing whether or not you’re a high-risk individual. It’s a pretty big group!
Will insurance cover the Covid vaccine for people who aren’t high risk and want it anyway? The jury is out on this one! We hope to have an update for you closer to fall. In the meantime, know that health insurers don’t dictate everything: Receiving the vaccine and paying out of pocket remains an option. This year, our vaccine cost will be $155, which is essentially our purchasing cost.
Nitrous Survey Update
We did not receive many responses in the affirmative for use of nitrous oxide in the office. For this reason, we won’t pursue purchasing the systems needed to administer it. Please be assured we still have multiple pain-control options for any in-office procedure.
Holiday Schedules
I will be out of town November 15–27. My staff will have access to me and be available for nursing appointments and questions, with medical coverage provided by my trusted colleagues as needed. When I return, and the holiday season gets busy, we will add extra office hours as needed.
A Member Writes
”Dr. Jahedi is the best! So attentive and very educational. She provides me updates on the latest studies and research of women’s health issues. I also adore her staff. Tommy the nurse is the bomb! I feel so comfortable with this practice.”
—Ryan L., patient